The avian influenza outbreak occurred in mid 2003 in South East Asia was the biggest and most serious one. The pathogen was confirmed to be A/H5N1 virus and there were 150 millions of birds being destroyed. While A/H5N1 virus was still an aggressive pathogen in Indonesia, Vietnam, Combodia, China, Thailand, and Laos..., there was an emerging human flu caused by A/H7N9 virus in late March 2013 in China.
AVIAN INFLUENZA A/H5N1 OUTBREAK SITUATION IN EARLY 2013
In January 2013, bird flu outbreak occurred in 2 household farms in Bau Tep hamlet, Tieu Thuan commune, Ben Cau district and Co Do hamlet, Binh Minh commune, Tay Ninh province. Total birds dead and destroyed in Tay Ninh were 3,438.
In Febuary 2013, there were over 10,000 infected chicken and ducks being destroyed in Khanh Hoa.
In March 2013, outbreak occurred in Binh Dinh, there were over 78,500 ducks being dead or destroyed.
According to Ca Mau Department of Animal Health, during the first 2 months of 2013 there were 3 outbreaks occurred in Tran Hoi commune (Tran Van Thoi district), Tan Phu commune (Thoi Binh district) and An Xuyen commune (Ca Mau City)...
In the same March of 2013, though there were not any A/H5N1 outbreaks confirmed in Dong Thap, there were 24/72 poultry samples from local markets showed positive results (33.3%). Moreover, there was a 4-year-old child who died confirmed to have been infected with this virus.
In April 2013, Regional animal health office No.6 coordinate with Ninh Thuan Department of Animal Health took samples from dead swallows which resulted in some H5N1 positive samples.
A/H5N1 AND H7N9 INFLUENZA SITUATION IN HUMAN WORLDWIDE
According to WHO, from 2003 to the end of 2012, there were 610 people in 15 countries being confirmed of A/H5N1, in which there were 360 death cases (59%). Indonesia was identified as the country with the most dead cases (160 people), followed by Vietnam with 61 dead people.
On March 31st 2013, Chinese government announced that 2 out of 3 people who acquired A/H7N9 had died. As of April 17th 2013, there were total 77 Chinese people got infected with A/H7N9 and 16 had died.
Though evidence of A/H7N9 human-to-human transmission hasn’t been confirmed by WHO specialists, some Hongkong specialists warned that this emerging avian influenza virus was far dangerous than A/H5N1 virus as those poultry infected with H7N9 were still healthy thus making it invisible. On the other hand, recently in China there is a 4-year-old child confirmed to be infected with H7N9 without showing any clinical signs and there are up to 40% of infected cases that did not make direct contact with poultry. This raises a question if the virus is able to mutate to transmit directly human-to-human.
H7N9 virus was believed not to infect human, and the most dangerous thing is there hasn’t been any vaccination against this disease.
VIRUS CARRIERS (RESEVOIR HOSTS)
Ø Muscovy duck (or musk duck): according to Alexander (2000), muscovy ducks acquire the avian influenza virus but do not show clinical signs except for mild diarrhea. The virus replicates in intestinal mucosa and vanishes after 4-5 days. The recovered ducks will become carriers and shed virus into environment.
Results from serology test of unvaccinated Muscovy ducks in Dong Thap showed positive rate of all flocks was 27.95% (Phan Mong Thu, 2012).
Ø Duck: Unvaccinated flocks showed positive results for A/H5N1 virus from 4.4-33.2% of samples. In Dong Thap this rate was 25%.
Ø Pheasants in Tien Giang and Binh Thuan were found positive for H5N1.
Ø Ministry of Agriculture and Rural Development recently announced that 2 samples collected in An Giang and Dong Thap were positive for H7 subtype virus (but this subtype was not similar to H7N9 virus in China).
Ø Swallow farms in Ninh Thuan were confirmed for H5N1 positive.
Ø Wild birds: a research in Alaska proved that more than 65% of aquatic fowls were H5N1 positive
Ø On April 9th, H7N1 was confirmed to be present in an ostrich farm in South Africa. This virus had been believed to be exotic to the country and being under a research of its relationship with H7N9.
Ø In China, H7N9 has been confirmed to infect pigeons, quails and chicken. Scientists are still working on tracking its root.
Ø Besides, other species like weasels, tigers (Thailand), panthers (Netherland) and cats are believed to carry this virus.
HOW DOES AVIAN INFLUENZA VIRUS TRANSMIT
Aquatic fowls and some migrating birds are resevoirs of AI virus (virus is present in saliva, nasal discharge, feces...) but do not show any clinical signs. The virus can survive off-host in the feces for at least 35 days at 4ºC and 6 days at 37ºC. Once invading birds, the virus mutates to high pathogenic strain and causes the outbreak. Those humans who make direct contact with infected poultry without proper protection may acquire this zoonotic disease.
AVIAN INFLUENZA A/H5N1 OUTBREAK SITUATION IN EARLY 2013
In January 2013, bird flu outbreak occurred in 2 household farms in Bau Tep hamlet, Tieu Thuan commune, Ben Cau district and Co Do hamlet, Binh Minh commune, Tay Ninh province. Total birds dead and destroyed in Tay Ninh were 3,438.
In Febuary 2013, there were over 10,000 infected chicken and ducks being destroyed in Khanh Hoa.
In March 2013, outbreak occurred in Binh Dinh, there were over 78,500 ducks being dead or destroyed.
According to Ca Mau Department of Animal Health, during the first 2 months of 2013 there were 3 outbreaks occurred in Tran Hoi commune (Tran Van Thoi district), Tan Phu commune (Thoi Binh district) and An Xuyen commune (Ca Mau City)...
In the same March of 2013, though there were not any A/H5N1 outbreaks confirmed in Dong Thap, there were 24/72 poultry samples from local markets showed positive results (33.3%). Moreover, there was a 4-year-old child who died confirmed to have been infected with this virus.
In April 2013, Regional animal health office No.6 coordinate with Ninh Thuan Department of Animal Health took samples from dead swallows which resulted in some H5N1 positive samples.
A/H5N1 AND H7N9 INFLUENZA SITUATION IN HUMAN WORLDWIDE
According to WHO, from 2003 to the end of 2012, there were 610 people in 15 countries being confirmed of A/H5N1, in which there were 360 death cases (59%). Indonesia was identified as the country with the most dead cases (160 people), followed by Vietnam with 61 dead people.
On March 31st 2013, Chinese government announced that 2 out of 3 people who acquired A/H7N9 had died. As of April 17th 2013, there were total 77 Chinese people got infected with A/H7N9 and 16 had died.
Though evidence of A/H7N9 human-to-human transmission hasn’t been confirmed by WHO specialists, some Hongkong specialists warned that this emerging avian influenza virus was far dangerous than A/H5N1 virus as those poultry infected with H7N9 were still healthy thus making it invisible. On the other hand, recently in China there is a 4-year-old child confirmed to be infected with H7N9 without showing any clinical signs and there are up to 40% of infected cases that did not make direct contact with poultry. This raises a question if the virus is able to mutate to transmit directly human-to-human.
H7N9 virus was believed not to infect human, and the most dangerous thing is there hasn’t been any vaccination against this disease.
VIRUS CARRIERS (RESEVOIR HOSTS)
Ø Muscovy duck (or musk duck): according to Alexander (2000), muscovy ducks acquire the avian influenza virus but do not show clinical signs except for mild diarrhea. The virus replicates in intestinal mucosa and vanishes after 4-5 days. The recovered ducks will become carriers and shed virus into environment.
Results from serology test of unvaccinated Muscovy ducks in Dong Thap showed positive rate of all flocks was 27.95% (Phan Mong Thu, 2012).
Ø Duck: Unvaccinated flocks showed positive results for A/H5N1 virus from 4.4-33.2% of samples. In Dong Thap this rate was 25%.
Ø Pheasants in Tien Giang and Binh Thuan were found positive for H5N1.
Ø Ministry of Agriculture and Rural Development recently announced that 2 samples collected in An Giang and Dong Thap were positive for H7 subtype virus (but this subtype was not similar to H7N9 virus in China).
Ø Swallow farms in Ninh Thuan were confirmed for H5N1 positive.
Ø Wild birds: a research in Alaska proved that more than 65% of aquatic fowls were H5N1 positive
Ø On April 9th, H7N1 was confirmed to be present in an ostrich farm in South Africa. This virus had been believed to be exotic to the country and being under a research of its relationship with H7N9.
Ø In China, H7N9 has been confirmed to infect pigeons, quails and chicken. Scientists are still working on tracking its root.
Ø Besides, other species like weasels, tigers (Thailand), panthers (Netherland) and cats are believed to carry this virus.
HOW DOES AVIAN INFLUENZA VIRUS TRANSMIT
Aquatic fowls and some migrating birds are resevoirs of AI virus (virus is present in saliva, nasal discharge, feces...) but do not show any clinical signs. The virus can survive off-host in the feces for at least 35 days at 4ºC and 6 days at 37ºC. Once invading birds, the virus mutates to high pathogenic strain and causes the outbreak. Those humans who make direct contact with infected poultry without proper protection may acquire this zoonotic disease.
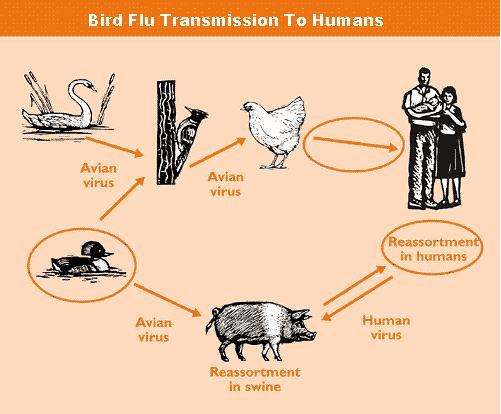 |
The virus invades the animal bodies via 2 pathways: respiratory and digestive (air, food, water)
- H5N1 virus was experimentally inoculated into a pig which later showed mild signs and did not transmit to other pigs
- When inoculated into the mouse, it acquired the disease then die.
- The result were the same when inoculated into the monkey
- In Febuary 2008, Thailand and France announced that they had detected H5N1 virus in the blood of mosquitos (this was the result of blood analysis on samples collected near H5N1 infected farms in Thailand, 2005)
- Japan announced the same thing happened in blood-sucking flies
- In 2010, Japanese scientists spotted a new strain of H5N1 virus which had mutated when it attacked pigs in Indonesia and turned into zoonosis.
- Pigs are capable of acquiring both influenza viruses from human and poultry so people believe that there is a new strain of virus undergoing such mutation that allows it infect human
PREVENTION IN POULTRY
1. Follow recommended vaccination schedule by veterinary offices
2. Perform periodical sanitation in farms (both inside and outside) with highly effective disinfectants like BIO-GUARD, BIOXIDE, BIODINE ®, BIOSEPT.
3. Provide good management and supply vitamins before stressful periods (changing weather, vaccination...) with BIO-AMINOSOL , BIO-VITA FORT, BIO-VITAMIN C 10% to enhance the resistance.
4. Restrict movement of outsiders, vehicles or other animals including wild birds into rearing areas
5. Infected poultry must be destroyed by incineration or deep burying. Do not throw carcasses onto fields, rivers or ponds.
6. Do not trade infected poultry
7. Do not import unauthorized poultry products through borderline.
8. Do not leave poultry free-ranged in areas that wild birds can get access to.
PREVENT TRANSMISSION TO HUMAN
1. Follow recommended vaccination schedule by veterinary offices
2. Perform periodical sanitation in farms (both inside and outside) with highly effective disinfectants like BIO-GUARD, BIOXIDE, BIODINE ®, BIOSEPT.
3. Provide good management and supply vitamins before stressful periods (changing weather, vaccination...) with BIO-AMINOSOL , BIO-VITA FORT, BIO-VITAMIN C 10% to enhance the resistance.
4. Restrict movement of outsiders, vehicles or other animals including wild birds into rearing areas
5. Infected poultry must be destroyed by incineration or deep burying. Do not throw carcasses onto fields, rivers or ponds.
6. Do not trade infected poultry
7. Do not import unauthorized poultry products through borderline.
8. Do not leave poultry free-ranged in areas that wild birds can get access to.
PREVENT TRANSMISSION TO HUMAN
- Avoid contact with infected or dead poultry
- Those who make contact with infected or dead poultry must wear safety-working clothes, boots, masks and gloves, after finishing wash with disinfectants
- Wash hands before and after contact with poultry
- Only eat well cooked meat, do not eat rare meat or blood soup
- Report to veterinary offices when detecting infected or dead poultry
CAN EGGS BE INFECTED?
- There are pieces of evidence that show H5N1 virus existence on the shells or inside infected eggs
- However, there is no case confirmed of being infected in human by consuming infected eggs
- In spite of being threatful, H5N1 virus can be destroyed by high temperature. Therefore, make sure to well cook the eggs.
CAN WATER SOURCES BE CONTAMINATED WITH INFLUENZA VIRUS
Rivers and ponds within outbreak areas can be contaminated with influenza virus carried by aquatic fowls and migrating birds, or by carcasses discarded by human.
- There is no human case suspected of acquiring H5N1 via water sources
- However, it is unsafe to drink from contaminted water sources. If there is no other source available, apply clorine and boil water before drinking.
CAUTION
Poultry infected with A/H5N1 and H7N9 can be subclinical (do no show clinical signs) so it is challenging to detect the disease. Besides, these viruses are zoonotic which can be transmitted to human. Therefore, prevention should always be on top priority and those methods above should be applied to provide optimal safety for human as well as poultry!
Poultry infected with A/H5N1 and H7N9 can be subclinical (do no show clinical signs) so it is challenging to detect the disease. Besides, these viruses are zoonotic which can be transmitted to human. Therefore, prevention should always be on top priority and those methods above should be applied to provide optimal safety for human as well as poultry!

 Hotline:
Hotline:

.jpg?width=120&height=90&mode=pad&anchor=auto&scale=both)








Comments